Skin Surgery
FSM PRACTITIONER WEBINAR
Carolyn McMakin, MA, DC

Download Slides
Download Handouts
Download Transcript
This transcript is computer generated. Listen to the audio.
(00:00:00):
Welcome to the skin surgery, FSM practitioner webinar postpone from last Friday. And you’ll see why you’ve got one set of slides. You got one set of slides. And I made some, I would say significant changes to them today. So my life as an FSM lab rat went to a new level. I got to a point where I just could not run skin anti-aging enough to keep the folds of my eyes from falling over. So people of a certain age, let’s say 73 have loose skin on their eyelids here. This is before and here. And this is after, right? Some of it is the man that he, but some of it is simply that you get tired of having blinders that block your peripheral vision. It’s enough of a problem that Medicare actually paid for the upper lid surgery. So these are some before and after examples.
(00:01:11):
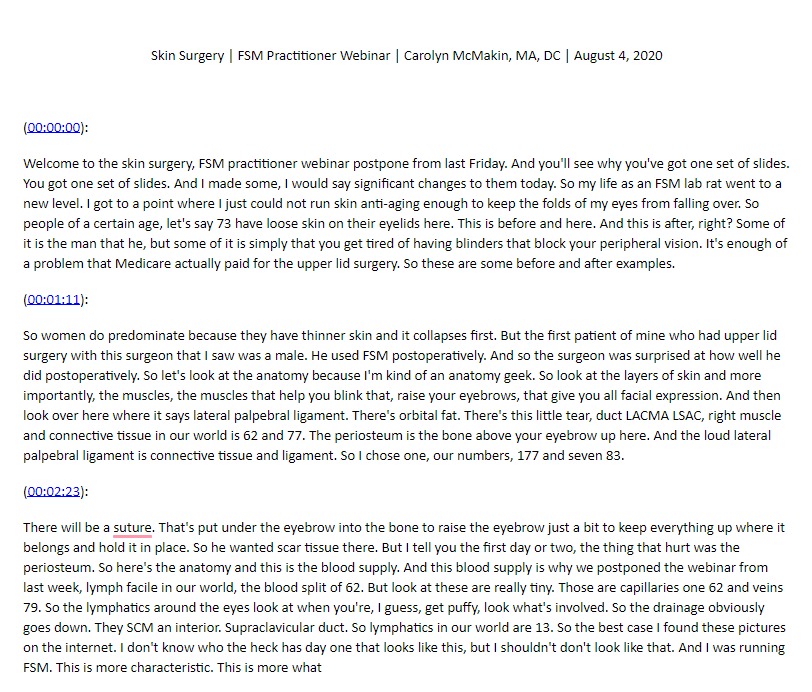
So women do predominate because they have thinner skin and it collapses first. But the first patient of mine who had upper lid surgery with this surgeon that I saw was a male. He used FSM postoperatively. And so the surgeon was surprised at how well he did postoperatively. So let’s look at the anatomy because I’m kind of an anatomy geek. So look at the layers of skin and more importantly, the muscles, the muscles that help you blink that, raise your eyebrows, that give you all facial expression. And then look over here where it says lateral palpebral ligament. There’s orbital fat. There’s this little tear, duct LACMA LSAC, right muscle and connective tissue in our world is 62 and 77. The periosteum is the bone above your eyebrow up here. And the loud lateral palpebral ligament is connective tissue and ligament. So I chose one, our numbers, 177 and seven 83.
(00:02:23):
There will be a suture. That’s put under the eyebrow into the bone to raise the eyebrow just a bit to keep everything up where it belongs and hold it in place. So he wanted scar tissue there. But I tell you the first day or two, the thing that hurt was the periosteum. So here’s the anatomy and this is the blood supply. And this blood supply is why we postponed the webinar from last week, lymph facile in our world, the blood split of 62. But look at these are really tiny. Those are capillaries one 62 and veins 79. So the lymphatics around the eyes look at when you’re, I guess, get puffy, look what’s involved. So the drainage obviously goes down. They SCM an interior. Supraclavicular duct. So lymphatics in our world are 13. So the best case I found these pictures on the internet. I don’t know who the heck has day one that looks like this, but I shouldn’t don’t look like that. And I was running FSM. This is more characteristic. This is more what
(00:03:32):
I look like it day, probably day one and two. This is what my dad looked like.
(00:03:38):
Think he got his eyes done, eyelids done. When he was 83 or four, he was a black eye. He was driving through Idaho and asked him to meet me for lunch. And he said, I can’t go out, but dad, it’s fine. No, I can’t go out. Come by the house. You’ll see. And he was totally black. He hadn’t even progressed to green and Brown, totally black from like all he had done, whereas eyelids, he didn’t have a facelift and him, it just, you catch a bleed and it drains all the way down. And then this way, this lady is the day, day three. So this is more common. When you look at the, when, if you look on the internet, now the procedure is actually they take a little fold. If you are my age, if you’re 25, don’t even think about it. Even if you’re 40, don’t think about it because you look great.
(00:04:36):
And none of this skin is loose. As we get older, this scan, I guess, stretches. Cause we blink so much. I don’t know what that’s about. And then the lower eyelid for me, I had the lower lid done because when I first started using a C-PAP it blocked those lymphatics and puffed him up and stretched all the skin. So the skin underneath was really loose. So there’s an incision in the upper land that goes like this and lower lid. Now, this is my surgeon. His name is Robert tower. He is board-certified in both ophthalmology and plastic reconstructive surgery, plastic reconstructive surgery is a very different discipline from cosmetic surgery. So he did this same surgery on two of my patients. And when he said, I would look as if X asked him, what’s it going to be like, when we’re done? And he said, Oh, you’re going to look like you’ve been in a bad bar fight.
(00:05:32):
And I looked at him and I said, no, I’m not going to bruise. I use frequency specific microcurrent. And he got real quiet, real fast. And he said you are that one? I said, yes, sir. I am. I’ve treated two of your patients. And their healing was remarkable. So I had his permission to use FSM immediately after the surgery. And the surgery is performed as an in-office procedure. So the day of the surgery, dr. Tower put the adhesive pads on as directed. He said, where do I put him? And I showed him where to put them on my forehead, red and green, right red on the right green on the left and the forehead black down below my collarbone. So you want it so that it will trace down to the lymphatic duct. Okay. So he secured the leads where he wanted them with tape.
(00:06:26):
So I said, you put them on. So you know where they are and then put the leads, the wires, where you want them and tape them in the back to keep them out of the way of the procedure. So I started skin postop day one before I left the building, I thought I wouldn’t bruise. Well, apparently the blood supply to the skin around the eye is a lot more robust than anything I had treated before. I had a fractured shoulder and George had fractured his hip and neither one of us bruised. And yeah, it wasn’t, it wasn’t pretty. You’ll see. What I didn’t know was that my electrolytes were off way off due to taking Lasix the morning of the surgery. I have many years and I wanted to keep the swelling down and that might’ve complicated things. It’s hard to know.
(00:07:30):
My potassium levels were 3.2. So the night of the surgery, I had just wicked leg cramps. We did a stat potassium on Friday and found out that the levels were 3.2. So that might have complicated things. It’s hard to tell. So the problem and why we postpone the webinars that I forgot the surgery at the age of 73 is different than the last surgery I had when I was 67. I didn’t bruise. I didn’t bruise. I made these slides today. No, spellchecking I didn’t bruise after six fractures in my left shoulder. So why would I bruise after a little eyelid surgery? Right? How bad could it be? Truth be told I was cavalier and a little bit arrogant and made promises to do a webinar the day after the surgery, figuring I wouldn’t bruise my mistake besides those is that I forgot the blood survive to the eye. I bruised a lot.
(00:08:32):
I’ll show you that picture on day two and a bit of permission from the surgeon. If you’re going to be treating postoperative patients, there has to be some version of a written permission from the surgeon or surgeons operating from, from the surgeon for surgeons operating in a hospital, whether you will stay in short date, short-stay day surgery, or as an inpatient verbal permission does not count. I’ve had two surgeons try and I didn’t let either one of them get away with it. No one will honor verbal permission. So my orthopedic surgeon said, yeah, sure, you can use it. And I said, no, Chris, dr. Hikes, no has to be in writing. And so on his permission, he wrote, okay to use where’d chiropractic electrical gadget. I said that’s just fine. And so when I didn’t bruise you, of course, attributed to his good surgical technique.
(00:09:37):
So some version of they will have postop instructions that they write for the hospital that has all their standard stuff, and they have a place in there to write down other things. So John Smith has my permission to use battery opera, tens device postoperatively for the management of postoperative pain. That is the only claim you can make. It needs to be obtained and signed at your preoperative visit by the surgeon. You have to have it in writing and it has to be done before you get to the hospital. Once you’ve gone for pre-op it’s, you’re done, you can’t get it signed. Then for every surgery, I’ve had, except for my open heart surgery, it has been a deal-breaker. It is required, or I will choose a different surgeon, no hard feelings, but this is my strong preference. And surgeons have always agreed. It is a tennis device and there are published papers on the benefits of using tens devices, postoperatively you or your patient needs to give the surgeon this information because it gives him cover.
(00:10:49):
It gives the surgeon, the medical and malpractice cover. He needs to allow you to use the tens device. It’s okay to mention the papers published papers, especially Dom’s, that’s the only thing we have in new injuries, but he won’t, he won’t care. It’s a tens unit. You can’t make any claims beyond the tens unit. We have nothing published in postoperative pain. So that’s the way that goes. Things to think about. Ask ahead of time, if you will be on cardiac monitoring. Sometimes this is unknowable and can be a surprise if you show up with an anomaly during surgery, but during the surgery, you’re always going to be monitored it’s after the surgery that they’re going to have you on monitoring if you have a cardiac problem. And the MicroCraft just totally scrambles the input-output to the monitors. So I was on monitoring during the surgery.
(00:11:52):
So I couldn’t use it during the surgery. I had Ivy anesthesia, pro propofol, I think they used and an anesthesiologist there plus dr. Tower. And they had me on cardiac monitoring during the procedure. Cause it’s an office thing. Be prepared to bring a program the CustomCare and a magnetic converter. The sticky pads are fine, but they’re not sterile. So they can’t be used in the, or you can use the magnetic converter once they’re back in their room. Even in a short stage, just put the magnetic pads under the, under the surgical area near the custom care causes, serious artifacts, and EKG monitors. The magnetic converter does not. And these days of COVID precautions, it will need to be sanitized and sealed and enclosed zip lock bag, put the pucks niche, separate bag. Most of the time, you or your patient will not be allowed to bring a guest during COVID events.
(00:12:57):
So we’ll make sure the postoperative protocols are first on your patients, custom care. So we have a custom care. You put the postoperative protocols that I’m going to show you during this webinar, you put those in your mode bank, you put them on the patient’s custom care in that order and make sure the patient or the patient’s caregiver knows how to use it. And they’re magnetic converter. We’ve got postop protocols for number, for different, a number of different kinds of surgeries. So the surgery was Thursday, July 30th at 9:00 AM and was expected to take three hours, took close to four. We used injectable anesthesia. He said, I wanted my COVID test did not come back by five o’clock the night before he said, we can do this under local with just some Advan. And I went, Oh man, okay. If I have to, but then my COVID test came back negative.
(00:13:53):
Yay. And so we could do the inhaled, the IB anesthesia. So we are modifying the upper and lower lips. It started the preoperative protocol the Monday before I’ll show you that the plan was for me to start FSM in the car on the way home and use ice packs. I, in fact, used ice packs, I think every hour, 20 minutes on 20 minutes off. In addition to the Fs, the FSM, I didn’t have any pain really. I took a quarter, so five, 1.2, five of oxycodone. So it kind of a little tiny chip at night when I went to sleep just to make sure the antibiotic medication, skin ointment, or provided pain meds, I never really had much in the way of pain preoperative plan was to remove lymphatic drainage. Right. And why would you need to do that? So I should have had a picture here of the, of the lymphatic system.
(00:14:59):
But if you remember that picture from a few slides ago, it got the lymph drainage all around the eye, down the face into the neck, and I’ve had so much C spine trauma, C spine surgery, open-heart surgery that it lymphatic scar tissue is a realistic possibility. So in patients that have had any neck trauma or neck surgeries I wrote a custom care protocol based in theory, and you can modify it any way you want. So there’s either 58 and then inflammation in the lymphatics to reduce the, and that was five minutes and it’s polarized positive. And then the basics then congestion chronic inflammation in the lymphatics scarring in lymphatics and look at the timing four minutes. So it’s not the lymphatics get their fluid from the veins. Both of these tissues are oneself thick. So lymph, the lymphatics, and the veins are right next to each other.
(00:16:07):
And they run in between layers of fascia. So you want all of these unglued, four minutes apiece. You want, don’t want the lymphatics to leak, tore, be torn and broken, right? And it’s a 36-minute protocol. I put it on myself with sticky pads at night. No, you can’t use a converter for this because your contacts are going to be on your forehead and on your chest. And you don’t want the magnetic pucks next year head. We’ve had a couple of problems with those. Oh, there it is. So there’s the picture. So that was the setup. There’s the lymphatics for the drainage to the head. And so you put the red on the right black cause you’ve got both sides to treat red cross black Christmas tree bumblebee, red cross black, right kitty corner. And I just branded at night laid supine in bed and with the head raise so that any gunk that was stuck in the lymphatics would come out and I laid there and mobilized the tissues and my neck and skin thing.
(00:17:17):
I did all this because the amount of swelling postoperatively was really impressive. So day one post-op run at two to four times on day one, I ran it continuously. So the two things that I changed there it is today, or I redid this program and this was 10 minutes, 10 minutes, five minutes, don’t stop bleeding. I changed it if I had to do it over again, this should have been done longer, but we’ll get to that. Then reduce inflammation because bleeding leads to inflammation. The frequencies that took the pain down were the ones to stop bleeding blood outside of blood vessels, stimulates classy pain fibers. And it is a deep diffuse kind of pain inflammation, torn and broken. And what right. Look at the pictures you have of the T of the anatomy. So in your slides, if you have those, think back to the anatomy is a lot of connective tissue, right?
(00:18:23):
What’s wrong with it? Well, it’s definitely torn and broken trauma paralysis, allergy reaction, inflammation, and vitality. Then that little pal people, ligament, he was so concerned about torn and broken trauma vitality in the ligaments. The current level is all at a hundred. And then those were just two minutes a piece I wasn’t too worried about them. And so this was mistake number one. So that protocol was a mistake. Number one, there was a lot of postoperative bleeding. So 1862 79, 60 twos, the artery, the capillary, the limp, the vein. That’s not lymph. That’s vain. What earth. Oh, well anyway, so I would do this. What I would, I would recommend is you change these times to 20 minutes each. Okay. then reduce inflammation, 200 broken, and connective tissue. So the bleeding was a problem. All alternating day. One postop goal is to stop the bleeding, turn down the inflammation, repair the connective tissue.
(00:19:39):
So I would recommend that you prepare a second unit with just 18. My, this protocol and my unit is identified with just skin postop 18 and it’s 18 and 62 arteries capillaries veins for 20 minutes, apiece arteries, capillaries veins, 20 minutes apiece. So it’s a, what is that? 2040 that’s a three-hour program, 18 and 62, one 62 and 79 for 20 minutes eat alternating, gentle. I use this more or less nonstop as a second set of pads. For three days, I wasn’t even two days. It was for three days. Every time I stopped running it, the pain would go up. Not horrible and the pain was never more than two or three, maybe a four, but it wasn’t that bad. But we put a second set of PE pads. So we had the big ones on my forehead that dr. [inaudible]
(00:20:49):
Put there. And I put the small ones, we cut down a two by two, put the small ones here right next to the, the big ones and hooked hook, second unit up. So you’ll see when we get to the pictures that it’s that I’ve got two sets of leads coming off my head on Saturday and Sunday supine in bed, he recommended that I sleep in a recliner and I actually am still sleeping in the recliner. It just is a lot easier. I’ve got one of those gliders that have electric recliner foot thing, and the head leans back and it’s been just comfortable to sleep in ice packs, medication as directed. So if your patient is they’re all going to be home, this is going to be day surgery. If your patient is at home, warn them ahead of time.
(00:21:46):
So to have their bed preps, that their head is up, they can put the head of their bed on, on risers. That’ll raise it up six inches. They do that for congestive heart failure patients and sleep, apnea patients. It’s good generally. Then the rest of it, look at the tissues. So you repeat stop bleeding, but if you have that second unit, you can use that to stop bleeding, the arteries, the capillaries, reduce inflammation, treating what torn and broken and the capillaries arteries, the periosteum. Alright, inflammation. We’ll look at the times. So if I had to do it over again, even though I have a second unit running the stop bleeding program, I would still run. I would still make this 20 minutes. It’s like the bruising was just incredible. The basics on the skin, but you don’t want to, you don’t want the skin to heal up too fast.
(00:22:49):
I forgot to put that other slide in there. I’ll, I’ll tell you next week, torn and broken in the lymph to reduce the swelling trauma and the lamp inflammation, congestion inflammation, and the fascia increased repair, increased creations in the fascia. And you look at the times, these are circled. That’s eight minutes. So it’s two and a half hours. Leave it off, take it off, go to the bathroom, run it again. I walked around with a customer care to customer care is one of my left pocket of my bathroom. And one on the right pocket of my bathroom day two postoperative, the times are shorter, right? So this is day one, it’s three hours. And if you add the extra time to stop bleeding, it’s going to be close to three and a half, two to four times in 24 hours.
(00:23:44):
Then stop bleeding, prevent bruising. Once again, here, I would change this and make these 20 minutes, especially if you don’t have a second unit instead of eight, eight, and five on arteries, capillaries, and veins make it 20, 20 and 20. Stop the bleeding treat inflammation, lymphatics, reduce the swelling congestion on the lymphatics, broken trauma paralysis, allergy reaction, reduce inflammation, then treat that little palpebral ligament. He was so worried about torn and broken in that ligament. Lots of time on connective tissue. If you look at the muscles in that anatomy and look at it, all these, all these insertions, there’s not a round ligament and the whole thing. There’s not a round tendon and the whole thing. It’s all connective tissue and blood vessels use two by two squares. Listen to what the doctor tells you when they say use ice.
(00:24:48):
That’s a good thing. 10 minutes instead of five, 10 minutes instead of five. And this is day two, still, you’re treating blood supply, reduce inflammation and the CA and bleeding 40 and one 16. You’re. There’s no reason for these to get infected. The immune system around the eye is very vigorous, very robust, and you will be given the patient will be given an antibiotic ointment to put around the eyes to the capillaries. Treat the skin increased secretions in the skin that keeps the skin moist times are shorter day to look at the times, increased secretions in the fascia. That’s longer, right? Inflammation in the periosteum. This was for Iran this whole day to protocol numerous times just to get inflammation. The periosteum, I never hooked up my precision care. Now I want you to notice down here, 81 and seven 83 is not there.
(00:25:56):
You don’t want to heal the periosteum too soon. They want it to scar. So 40 and seven 83 is okay for comfort and to reduce swelling, but increasing secretions than periostin didn’t seem like a good idea to me. So I didn’t do it, but you can, if you want and give it a try and see if it turns out better, but that was my logic in why 81 and seven 83 wasn’t there. So Monday mistake number two was I was really bruised a day two. So I ran a few minutes of day four that included two minutes, each of two 84 blood clots in the arteries and the capillaries that made my left eye start bleeding again, which is kind of gross, but you have a little sterile two by two gauze pads, the whole box of them. And you pad the, absorb the liquid away with that.
(00:26:54):
And as spread the bruising down my face to about halfway down my cheeks and turn my cheeks, we’ll see when we get to the pictures is a good idea, in the long run, is kind of bad timing. So I went backdate two or three days three, I think back to 18 and 62 all day again. And when I, it says day four, it probably really means day four, really? But yeah, that was a mistake. Number two. Remember I told you during the core that I would warn you about every mistake I ever made. Okay, well, they’re here. You get to see them in a lifetime. So stop the bleeding again. Now, this is day three. The times are shorter, but this in some of the channel lays are eliminated. You don’t have to do trauma paralysis, allergy, or action with every tissue. It’s 93 minutes.
(00:27:47):
So it’s shorter. Is it two to four times in 24 hours? I was running, I was running it constantly. I ran FSM probably 10 hours, 12 hours a day. Take time off in between just to let the tissues rest a bit. Cause you’re driving. I’m pretty hard to recover up to six hours out of 24 hour. Stay hydrated, increase your protein and vitamin C now, because my potassium was 3.2, when 3.6 is normal, they got kind of excited. And my daughter’s a nurse, almost a nurse, and she said, potatoes are the highest source of potassium. So I ate potatoes and bananas. I ate, I didn’t think it was possible. I hate red potatoes for dinner, breakfast, lunch, and dinner. And Sunday, I couldn’t look at a potato, but I had one meal that was potatoes and took my potassium two in the morning.
(00:28:51):
And Monday, my potassium was 3.9. So I got extra points for that. Anyway, you’re still on day three, you’re stopping bleeding. I would run this. If you don’t have a second unit, run it at least 10 minutes. The bleeding causes pain, inflammation, torn and broken. Now this run look at the time, pay attention. The time this runs longer, it could have run longer, but I didn’t want the protocol to go too long. Inflammation, vitality, torn, and broken that little ligament. They artery the capital areas. If you look how well-vascularized it is, these are just all the basics for the most important issues. Postoperative user patent set up sticky pads on the forehead. You’ll see the pictures right then increased secretions in the skin. So you want the skin secretions and vitality to increase. Those are four minutes, a piece three 55 is the skin one 40 twos.
(00:29:57):
The fascia, once again, you’re increasing ground substance. We think by increasing secretions and fascia, then torn and broken a periosteum inflammation, the periosteum vitality, and the periosteum times aren’t too long, but I didn’t want this. I will didn’t want the protocol to be too long. Day four. So day four was the one that I ran on day two that dissolve the blood clots. So that was kind of a thing. And that was only four minutes apiece. And it was enough to stop the bleeding on date to start the bleeding again on day two. So yeah, at the dissolve blood clots thing really works, reduce inflammation, support vitality, what tissues, the blood supply inflammation and the immune system, 40 a month, 16 40 and 62 77 is connected tissue. The ligaments 100. What are we doing? What’s wrong with the ligaments, torn and broken.
(00:30:59):
That makes them inflamed. Then vitality. Any of these times you can adjust based on what you think about it. Blood supply, that’s the muscle bellies that you saw 40 and one 16. And then the capillaries that he said pads up is repeated over and over again. They for postop. So it’s all still gentle. And the times are shorter and more of the channel. Aes are eliminated and some new channel is so secrete, ground substance increased secretions of fascia 81 and 73, seven 83. You know, that is there. So by day four, it’s just fine to get the periosteum. It’s like, okay, time to go to work. Let’s rebuild this whole. They put in the bone, they put a little stitch through it and they want it to scar. Now at day four, you’ve run enough microcurrent that you could do that. Now, not everybody is going to sit at home on their own customer care and run this all day.
(00:32:04):
It’s too intimidating for most people. I got to tell you, you don’t feel like going much of anywhere. So you could, you could either sell the paint, put this on the patient’s custom care they already have, or have them come into your office and just park them someplace. If you have a recliner somewhere, you can just park them in your office and just run this once a day, they will heal faster than they would normally heal. It would be worth the trip for them. If you can put it on their own custom care, if you can trust them to run it, that would be a thing. Now I created a program for lymph drainage. This was the original one inflammation, congestion infection, 60 61 66. One of these is strap. One of these is staph. I can never remember which one is which, and you notice those infection frequencies are two minutes a piece, and then vitality in the length.
(00:33:03):
That’s two minutes. So I’m modified the lymph drain is a swelling around the eyes. It doesn’t take a lot of swelling in the eyes to make it feel really puffy and make it difficult to open your eyelids. You’ll see. So look at the times are different between the two. I started out with four minutes, four minutes, and then two, and this is 10 minutes on 40 inflammation in the lamp congestion on lamp five on the infection, frequencies two on these the one and the two frequencies. Cause I don’t have any evidence that they work and I don’t like messing with the [inaudible] system and then vitality and the lymph has polarized positive from the top of your forehead down to your collarbone. So surgical systemic is a program that Mary Ellen Chalmers wrote for her patients who have dental surgeries. And she runs it during the surgery on a magnetic converter or custom care during the surgery.
(00:34:09):
So these, because she does a lot of demo work on patients that have root canals and osteonecrosis, she doesn’t do the surgeries, but she sends them with the custom care and her oral surgeon runs this during the surgery. So look at it. It’s like the basic basics of the concussion protocol. So 94 94. And then you want to just, just do a drive-by notice. These are all only one minute apiece, just do a drive by on the pituitary to keep it functioning so that it doesn’t fall asleep due to trauma, and then treat the adrenals. What are you doing to do the basics? Leaking basics, remove anti-seizure remove toxicity, support secretions to keep the inflammation down and vitality and the adrenals, and then do all the same things for the liver. Treat the liver for inflammation, chronic inflammation scarring treat the liver for toxicity and anesthesia.
(00:35:11):
Now you notice it because people have anesthesia during any kind of surgery. This surgical systemic is designed to do inflammation and toxicity in the liver and then do the kidneys. So what are the organs that are clearing, especially Ivy anesthesia, which is what you use during jaw surgery and during skin surgery. And I have to tell you, I run this by running this on my custom care. So I had the sticky pads on my forehead and two custom carers, one on each side of me, I had the surgical systemic programmed on a separate custom care. I don’t even know how long this thing runs. I forgot to look it up, but you can do the math. I ran it probably twice a day. The first two, three days felt pretty crummy, but we were still working on the electrolytes, stopped bleeding.
(00:36:14):
This is what I, and this is what I switched to on the second unit when I had dissolve the clots. So this is just 10 minutes. Each the thing runs for what is that? 30, 60, 92 hours. So this ran for two hours and I ran it pretty much nonstop for two, three days. Now, the other day, when I was ready to start dissolve the bruising. And you’ll see when I you’ll be able to tell when I started doing that what’s today, Tuesday. So probably Sunday. It was time to get the bruising out of my eyes. And so I did two 84. Now what I didn’t hadn’t thought of until I experienced it was blood clots clog up your tear duct. So 20 ones tear doc, the skin bruise three 55, the blood supply, obviously blues 62, the lymphatics had blood clots in them and the fascia and then inflammation, congestion, and vitality, and the lymphatics everything’s alternating except for inflammation, congestion, vitality, that’s all polarized positive from the top of your head to below your collarbone.
(00:37:36):
And that I ran, I put on, I was down to one custom care, I think as a Sunday, maybe yesterday. So what else do you do modify these programs, protocols, depending on patient’s condition and response to treatment. So if they have Ehlers, Danlos are they’re really flexible. Increase the amount of time on one 24 and 77. And I mean increase it. Don’t be afraid to make these programs along these patients. Aren’t going to be up walking around. It’s just, they are number one. They are ordered not to walk around. You are not to get your heart rate up. You are not to lift anything. You are not to walk or hike or do anything. I would say a surgeon would say, don’t do anything stupid. If they have thins scrap, fragile skin increased the times on three 55. If there’s bruising, as you saw increase the time in 24, make sure the diet is clean.
(00:38:35):
No wheat, that’s not wet. W a T T that’s w H T reduce the inflammatory food for two to six weeks increase the quality of protein. So in person pretty much I’ve had potatoes and fish increased vitamin C concussion every day, at least once. And I tell you, I don’t eat potatoes, didn’t eat potatoes because they have a glycemic index of like one it’s like getting right white rice or just straight sugar, right in the time between I had, when I had my blood work done a week ago and it was normal. And the blood work done on Friday when the potassium was super low. And then the blood work done on Monday to check on the potassium between Friday and Monday, my fasting blood sugar went from one 45 to 96, eating potatoes three times a day. I do not understand that anybody want to let me know if you understand it, that would be great.
(00:39:38):
Do not run concussion in Vegas, do not stimulate the Vegas at all. It suppresses the immune system and with all this bleeding and torn tissue, the Vegas is going to be turned off and it just needs to be turned off. That’s just how that goes. Ran concussion protocol all the time. And that’s part of the surgical systemic around brain fog with increased time on remove anesthesia that I forgot to put in, but I increased the time on remove anesthesia and toxicity. I didn’t run it once a day for four days. I didn’t run it at all until Sunday and just leave everything else alone. Don’t manipulate everything. Anything else use FSM just to heal this thing. We’re going to go in and treat scar tissue in fibrosis at week eight and the scar tissue needs to be really solid. So I’m going to use probably 51 and not 13, but I’ll do fibrosis and the fascia, the blood supply, and the lymph.
(00:40:38):
So over-optimism was based on my experience. Scheduling this webinar for Friday, didn’t anticipate my low potassium. But it was based on my experience using FSM postoperatively. So many times Terrell Owens, no bruising, no swelling, no pain. Hip surgery is no bruising. My horrible shoulder fraction never bruised breast reduction, tummy tuck on a patient, no bruising nine jaw surgeries on me, no bruising, no swelling, no pain. All patients treated postoperatively, Halley celebrated healing. So I hope that I can make it through this. And I look as good as I think I will. Yeah, that ship sailed. If anything goes badly, Kevin we’ll cancel the webinar and we’ll catch up next week at the same time. And the next slide actually is a photo sequence. So this was the first day. This was Thursday. So look at bruising around my eyes. That was the first day.
(00:41:37):
And my eyes are not quite open because they couldn’t, they were really swollen. You can see it more on this lid because it was near the window. And you notice already that my cheeks are even fuller than they usually are because the lymphatic drainage, just all that fluid from the surgical intervention has to go someplace. And at this point, this is day one where I have only one pad by day two. There’s a second pad that you can’t see, but there’s the two red leaves. There’s the two green leads. So on day two, we’d put a second on Friday, we put a second set of pads in there to stop the bleeding and take out the swelling. Yeah, it really did feel as miserable as I looked. But this was day three. This is Saturday and the bruising is already swelling, slowing down a lot of puffing and bruising under the skin under the eye day four.
(00:42:41):
This was Sunday. And you can see the swelling down here is down the left eye on the right eye were completely different in nature Monday. This is when Danielle, so this is the PDI supply closet. This is when Danielle came in and when I dissolved, see this, remember on day four, I started dissolving the blood clots with some and bruising with some seriousness. So you can see here that the bruising is spread further down my face. That happened on day two. When I ran that for just four minutes, the clot started the bruising started dissolving up there Monday. I look like that. And this is today. Almost no swelling, a little bit left. I’m gonna see these are still my stereo strips. So there’s still bruising under those. This is a picture in my dining room that, that gentlemen is the last kahuna on the big Island of Hawaii part of that lineage.
(00:43:46):
And so that’s, that’s our dining room office. So the FSM and PDI offices are in the in my house. So that’s today. So I’m hoping you get the drift and this will help. There are a lot of people my age, your age, maybe that have this procedure and it is not an Aqua and innocuous under normal circumstances. I would have looked like that for about a week. He said, I would look like I was in a bad part bar fight for six weeks. I expect him to be pleasantly surprised tomorrow when I see him. So this has made a day, the stairs strips will come off tomorrow. We’re doing a followup webinar next week. It’ll be short. It won’t be a full hour unless I find something else to talk about. Imagine that. So we’ll be back. What day is that scheduled for?
(00:44:44):
Okay, so next Friday. So it’ll be, today is Tuesday. And the first day we had available to do this would be next Friday at four o’clock. So the basic principles are what you can apply to anything that you do to treat a patient postoperatively. Not all patients will have the ability to do what I did and treat with one or two machines full time for basically five days. And, but I have a vested interest in this. I just really wanted to knock the surgeon socks off and we’ll see, we’ll see what he says. We have exciting news resonance effect was adopted or approved by North Atlantic Books and Pentagon Ram random house as an audiobook it’s available on audible for pre-purchase. Yay. That comes out August 8th. I think remember the thousand dollar publication prize, it’s a cash reward to any practitioner who publishes any paper of any sort in a peer-reviewed journal about the use of FSM and any clinical condition.
(00:46:01):
This is presented yearly at the events. I’m figured out what we’re going to do next year when we’re sort of socially distance. And there’s only a hundred of us instead of 200, but we’ll figure that out. We’ll fund the statistical analysis. The methods section, the payment is just acknowledgment, but it helps compensate for the writing effort. Those of you that are in professions like chiropractic physical therapy, occupational therapy, osteopathy, almost any profession that has, a journal will accept papers from their members and publish papers. And the only way we’re going to progress. And I’m just saying, it’s a reality check. I’m 73 years old, I’ve published what, 10 papers. I’ve never published a paper before 1998. And I’ve done them all collected case reports of the lowest life form, but they do count as evidence-based medicine. So what I did in this postoperative stuff has never happened until somebody publishes it. And yeah, I know I should probably publish it and I’ll see if I can talk the surgeon into helping me out with that. But the truth of the matter is the future of FSM is in your hand. So I got us this far
(00:47:22):
And I’ll be around for a while
(00:47:24):
For sure, but the future of FSM is in your, so if you enjoy what we do, you enjoy what you do and you want it to become more widely known than the more acceptable we have to publish papers. It’s worth the pain. Trust me. We’re going to do a live stream five-day core August 24, 25, 26, 27, 28. It is the best of module one and module two. So basically module one is the pain and injury module. It’s for three days. Module two is the neuro and visceral module. And I’m going to take out the redundant material, what is in each of them a little bit and take those six days and come and clean, take out the redundant stuff and combine it into a single five day. It’ll be 9:00 AM to 6:00 PM Pacific standard time as a Livestream we have patient demos that I’m really excited about.
(00:48:22):
Some really difficult and interesting patients. And it, I think it will be fun and pain. An injury module is competitors Maine. We had a great time before. This is our second one. And so this will be September 18, 19 and 20 9:00 AM to 6:00 PM Pacific standard time. It is going to the best of both worlds. We just have a ball doing this and the neuro-visceral module, we probably, I don’t think we are planning to film that live. At least we don’t have a commitment to do that. And then the advanced is going to be interesting, kind of depends on what this epidemic does. February 17th, 18, 19 2021 is five days. So I will do the five-day course seminar that is also going to be live stream in February. We have videographers in Arizona that will come and tape it FSM sports to be the 22nd and 23rd sports masterclass.
(00:49:24):
Kim has gotten far enough that there are enough of you that have taken our course, that she’s going to do a small group masterclass on somebody, probably professional athletes. I’m not sure who she’s coming is getting his patients, but she’s got just amazing training as an osteopath. She has her license as a massage therapist, but she was taught osteopathy. So this is osteopathic massage. It’s amazing. The Advanced is going to be February 25th and 26th. It’s the usual magical advanced. We’re going to have it at the same place in Phoenix, that hotel did survive the lockdown they are surviving. Now during the Arizona spike, the plan is to have it in that same ballroom. It will be limited in person. So normally chairs are three feet apart. These are going to be six feet apart. So instead of being able to take 200, as we planned, we will be able to put 100 live in the ballroom.
(00:50:32):
Mass will be required or negative COVID tests have to be provided to the FSM registration. I’m not sure how we can monitor that. And I see the first time Kevin has heard about that. So we’ll see the hotel is arranged to change their food service. So they have safely, safely served food, try saving, saying that at five o’clock at night, at the end of an interesting week safely served food and we will live stream the advanced we have, I have the some of the speakers already arranged. I’ll start doing that. The symposium, Jim Oshman, Jerry Pollack, Jim Turner, there’s Mary Ellen Chalmers is going to do 90 minutes. That one, I do know at the advanced she’s just finished a master’s degree. Like she’s a dentist and a nature path, and she didn’t have enough to do so. She went and got a master’s and had neck, I think had neck pain management at UCLA.
(00:51:35):
So she is going to do a 90-minute workshop at the advanced and that I am, I’ll be in the front row. I’m six feet back. Of course. Jim Turner, John Sharkey is, I don’t see how they’re going to come. If any of these, these symposium speakers cannot or choose not to come in person. We will have them videotaped at home. And then we’ll take that. We’ll send videographers to their homes. They will tape their presentation and send us the film and we’ll play it live on that day. That will be the usual practitioner case reports. I’m going to start stalking people pretty soon. So if you have case reports for the symposium, that would be a good thing. And then March 1st and instructor training, and I’m not sure how we’re going to do that. We’ll have to figure that out. It will be limited 10 people, everybody, a warm mass.
(00:52:30):
This fires is a real thing. So for our we’re all good and healthy. So that’s been kind of fun. So this is what we do. You guys, this one surgeon, and pretty much every surgeon that we’ve ever dealt with, who’s seen a postoperative patient, changes their mind about what is possible changing medicine, but we are going to do it one patient at a time until we get published papers. And until we get control trial isn’t until we get just a lot further down the road in 10 or 15 years you can’t change medicine wholesale, but you can change the mind, change the mind of one physician by treating one patient or even being that patient. As I did this time, changing lives one practitioner at a time, every single person, how many people are signed up for this thing, 300 and some of you there’s 300 and some odd people that will see this and know what to do 104 people on their 330 something registered.
(00:53:41):
So they’re the 300 and some odd of you that will be able to treat postoperative patients with this kind of foresight and at least a recipe, at least a way to look at it. My job, as you’ll find, when you start doing the, the modules and the when you start doing the modules and even the five days, my job is to teach you to think 20 years ago, I thought my job was to teach you frequencies and how they work. We know how to do that. Now my job is to teach you how to think about how to do what it is you need to do to correct the cause of what is happening in front of you. And I didn’t make a point of that during this webinar, but that’s, that’s what you’re going to find in the modules. That’s what you’re going to find in the five-day live stream.
(00:54:38):
We’ll have a special price. I am sure for repeat attendees and then changing even one patient’s life changes the world, and that’s what you guys are doing. That’s the thing that just is breathtaking. When I think about it changing even one patient’s life can change the world. So the patients I’ve treated postoperatively, the patients you’ve treated for pain, low back pain, any patient you treat when you change that patient’s life. When you give them hope, when you give them pain relief, when you give them a vision of what is possible, that ends up changing their world. And that changes our world. So on that note, I think we’re going to do, are we going to do Q and a? Do we have QA? We have questions. Read them to me. Okay. All right. Wondering about bad placement on pads placed on the front of the body frequencies.
(00:55:35):
Only address the skin, you guys Sherry. Everybody. I showed pictures of where the pads go. All four on the front. Oh, this came out before that. Okay. Yeah. Sorry. Yeah. There’s two at the forehead and then two under the, the two at the sternum to treat the lymphatics. So yeah,, those pictures are where I put them. So the concerns about placing the magnetic converter next to your head. Yeah. Concerns about placing the magnetic converter next year. He had, I don’t put it there because the brain is sensitive to magnetic fields. That’s the first thing. And we had one practitioner on the page that made quite a fuss about the fact that she put the magnetic pucks next to her head and had all these side effects and whatever. So I don’t know what she was reacting to, but just on the off chance, let’s not do that.
(00:56:36):
You can do just about anything you need to do, especially when you’re putting the pen, when you’re treating things like surgical, systemic, or customcare, Richard, Luke, and gay bless you. Okay. Under Armour drink P light for the potassium cramps, a better source of potatoes. This stuff really works. I know that I’m a crammer. Yeah, that’s for sure. Well, the only challenge I have rich with the PD light, it was, well, it tastes disgusting. The pills, the, I think it was 50 million equivalents. I don’t remember. It was a prescription dose of potassium. I took that for three days. And from now on any time I take a Lasix, I will be taking potassium, but take it from red shoes. Got cramps. How nice to hear from you? That’s lovely, William, right? Where is the magnetic for the surgical systemic?
(00:57:37):
During the actual surgery, if you’re allowed to use them during the surgery, you put them by your side. I did not use them during the surgery. I used them when I got home and I didn’t figure out that I needed them until Friday. So I programmed a second unit. As soon as I could see, well enough to, to program a custom care and rich Lukin gay, I don’t, he would be able to explain this. My, my vision cleared up there is an Iran, lymphatic drainage post-op. And the reason I ran that so much was my vision would get all blurry. And as soon as I ran lymph drainage, it would clear up. So every time I got tired of not being able to see, I would run lymphatic drainage and the fluid bid out, Sherry who good. I’m glad I didn’t hurt your feelings.
(00:58:22):
Cold potatoes do not raise blood sugar. Well, he was hot with lots of salt because my sodium was low as well but okay. It’s nice to know the cold potatoes. I don’t know. Don’t raise blood pressure. A question about pain. Yeah, no, Nope, Nope. I have no pain. Like my pain has been like a two or three, which at my age, just doesn’t count as pain. You get above the four or five, then you, you know, mind. But I only took like this little teeny chip of a five milligrams, so we cut it in half. So that’s two and a half one in 1.2, five of oxycodone. I can’t take Percocet or Vicodin or any of those with can’t take Percocet or Vicodin. So we just use straight oxycodone and put one, 2.2 fab, which is like a homeopathic dose. It just helped help sleep.
(00:59:17):
Come on. But that’s a good question. No, I, I really didn’t have any pain. It’s if you stop the bleeding, there’s no pain. And every time I stopped running, stopping bleeding, my pain would bump up to a four, four and a half. A symposium will be live stream. We will do that. I’m not like anybody we’ll get on planes. Can we get copies of the slides? Yes. I’m afraid as I was changing sides today, Kevin said I already sent those out. So at teal, send them out tomorrow and just be a dropbox. I finished that. I finished the slides at three 47 today. And Jeff Bruno, any additional recommendations for knee surgery? Yes. We have postoperative protocols for knee and hip. I think they’re in the mode bank, surgical suite. I think you look good. Lord chicken. We need a pre-op picture. Oh, you know what?
(01:00:14):
Dr. Tower took that and he said, he’d give it to me. So next week, when we, when we revisit this I’ll, I’ll do the preop and it was bad enough that they, it was bad enough that Medicare paid for the uppers. I had to pay for the lowers, but that was to Ben. Oh, why does, how Christina, how nice this is so cool. I love it. When you guys ask questions, I’m really missing you all. This is really anyway. Nevermind. No whining. You positive on the lymphatics because the lymphatics like to be polarized. For some reason, I’ve always used polarized positive on the lift even in the head, but when you’re doing lymphedema, neck defeat for general lymphedema, you always polarize it positive. It just loves it. I just loved being polarized. It just works better. Oh, Alfred, thank you very much for all the data.
(01:01:09):
Oh, well you’re welcome. Do good things. That’s the, that’s the thing be the remainder of your healing. Thank you very much. I will be so glad to get these surges strips off. They’re driving me crazy. I can’t open my eyes. Well, we’ll see what he says. I will see you guys next week. I’m looking forward to them already. I promise I’ll make slides before the day of, but it’s really been an interesting Oh, Hey, it’s good to hear you too. It’s yeah, so it’s been really nice getting to talk to you. We will revisit this next week and I’ll let you know how the week comes out. Then, we take pictures just about every day, so have a good tomorrow and I’ll see you next week. Love you. Bye.
