Vestibular injuries are often undiagnosed but can have devastating impacts on patients’ quality of life. These injuries require careful screening and assessment, as patients rarely present with an explicit vestibular diagnosis.
Why Vestibular Injuries Matter:
- The brain relies on three key systems for spatial awareness: the vestibular system in the ears, visual input, and mechanical receptors at C1-C2 and lower extremity joints
- When vestibular injury occurs, the brain compensates by relying more heavily on visual and mechanical inputs
- This compensation can lead to numerous challenging symptoms and functional limitations
Common Symptoms:
- Difficulty in visually complex environments (malls, grocery stores, warehouse stores)
- Problems with reading and computer work
- Memory loss and cognitive difficulties
- Anxiety or “panic attacks” (especially in busy places)
- Balance and coordination issues
- Dizziness, disequilibrium, nausea
- Symptoms may worsen with changes in air pressure
- Sleep disturbances and night-time panic
- Feeling of fullness in one or both ears
- Heightened sensitivity to sounds
Screening and Assessment:
- Key History Questions:
- Experience of dizziness, nausea, disorientation or disequilibrium
- Difficulty with balance or coordination
- Anxiety in busy/crowded places
- Issues with moving visual information
- Sleep disruption patterns
- Memory or sequencing difficulties
- Symptom changes with weather/pressure changes
BIVSS Vestibular Injury Assessment Questionnaire:
Visual System Symptom Questionnaire 18
- Key History Questions:
- Experience of dizziness, nausea, disorientation or disequilibrium
- Difficulty with balance or coordination
- Anxiety in busy/crowded places
- Issues with moving visual information
- Sleep disruption patterns
- Memory or sequencing difficulties
- Symptom changes with weather/pressure changes
Treatment Approaches:
- FSM Protocols:
- Careful screening before using 94/94 frequency
- Monitor for adverse reactions
- Consider use of Meclizine if needed
- Modify treatment approach based on patient response
- Additional Interventions:
- Neuro-optometry referral (FCOVD) for prism lenses
- Vestibular rehabilitation (after 3-6 months of prism use)
- Medication management as needed
- Environmental modifications
- Sleep adaptations (night light, positioning)
- Create visual horizons in environment
Cautions and Considerations:
- Approximately 10% of vestibular patients may experience adverse reactions to 94/94 frequency
- Consider Meclizine (25mg) for symptom management
- Progressive lenses are not recommended
- Condition requires ongoing management rather than cure
Patient Education Resources:
- vestibular.org (VEDA)
- Support group information
- Lifestyle modification guidelines
- Home adaptation recommendations
Information about Vestibular Injuries for Patients
The vestibular system gives your brain information about where it is in space. “My location in space” is so important to your brain that is has information from three systems that all has to agree before the brain will do anything else easily.
Both inner ears have three semicircular canals, shown in the picture below. Each semicircular canal has a different orientation, horizontal, vertical and diagonal. Each canal can give the brain information about where the ear is in space. The two ears have to agree with each other or the brain gets conflicting information.
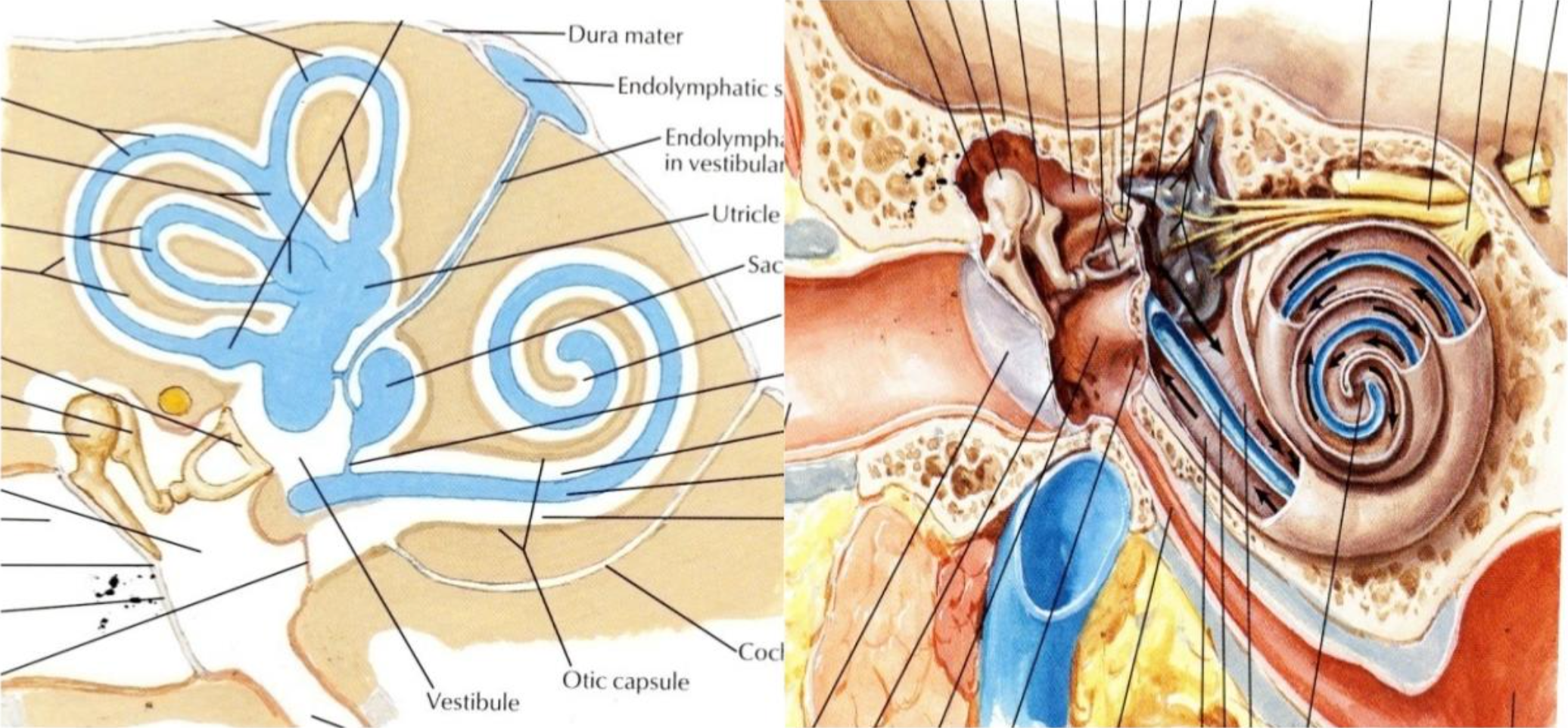
The semicircular canals in the ears control the smooth tracking of the eyes from side to side. We take this smooth tracking for granted because we use it all the time for things like reading, scanning from side to side as we walk, ride a bicycle or ride or drive in a car.
The second source of “where am I in space” information for the brain comes from the eyes. The eyes should be on a horizontal line so the brain can find a horizon to orient itself in space.
The third source of information is the position receptors, called proprioceptors, in the joints in the upper neck, the hips, knees, ankle and feet.
The information from all three of these sources has to agree or the brain doesn’t work correctly. If one ear has been injured, the brain learns that the ears don’t agree with the eyes and the joints and it learns to ignore the ears during the day. At night, when you’re asleep, your eyes are closed and the joint receptors don’t work because you’re laying down and they don’t have any input from gravity. At night your brain has only input from your ears, the two ears disagree about where you are in space and this creates the problems when you’re asleep.
Symptoms from Vestibular Injuries
Anxiety: The most primitive part of the brain needs to know where it is in space before it will allow the brain to do anything else. When the input from the eyes, the ears (semi-circular canals) and the joint receptors don’t agree this primitive part of the brain becomes distresses or fearful and the person experiences this as “anxiety”.
Fatigue: Because simple every day activities require so much effort, vestibular injury patients can experience extreme fatigue that can be mis diagnosed as “chronic fatigue”
Disequilibrium: Patients with mild vestibular injuries aren’t usually dizzy. They feel slightly off balance, as if their body isn’t sure about where it is in space. The best description for this is “dis-equilibrium”. The patient
can occasionally bump into things or stumble over something because they aren’t sure where their body is in space. Some patients describe it as feeling off balance.
Balance: Vestibular patients depend on their eyes for balance and have trouble with balance when the eyes are closed or busy processing other visual information that requires the eyes to move from side to side. This can make activities like riding a bicycle, roller skating, skiing or even walking difficult or impossible.
Light sensitivity: There is a strong neurological connection between the vestibular system and the eyes. For some reason vestibular injuries make the eyes very sensitive to fluorescent lights.
Trouble Reading: The vestibular system controls the smooth movement of the eyes from side to side. When the inner ear has been injured the eyes tend to bounce as they move from left to right across a line of text in a book or on a computer screen. The patient isn’t usually aware that the eyes are bouncing; they just know that reading makes them tired, or gives them a headache or they notice that they have to read the same line of text multiple times to absorb the meaning. And it may take them a few years to notice that they don’t read for pleasure any more.
Memory Problems: The vestibular system participates in cognitive function and the movement of information from short term to intermediate term to long term memory. Patients with vestibular injuries may forget conversations or parts of conversations and just assume that they have “early cognitive decline”. Some patients will forget days or parts of days and have concerns about brain function or may even fear that they are schizophrenic. They tend to leave items out on counter tops because, if they put the item in a drawer they can’t remember where it is and have trouble finding it, or even remembering that they have it. They specifically have problems with sequencing activities and memory for numbers and names.
Busy Crowded Places: The brain learns to ignore the ears and depends on the eyes for information about where it is in space because one ear tells it one thing and the other ear tells it something else. Because the brain has learned to ignore the ears and depends only on the eyes for information about where it is in space, the eyes must be able to find a horizon. The eyes also have difficulty telling the brain about “position in space” when they are busy looking at lots of moving objects. Vestibular patients get anxious in airports, warehouse shopping facilities like Costco or Sam’s club, large grocery stores or “Big Box” variety stores and multi-level places like a mall. Some patients have been mis-diagnosed with a psychological condition called “agoraphobia” or fear of open or busy spaces when they really have a vestibular injury
Barometric pressure: When the inner ear has been injured the thin membrane that separates it from outside air pressure, the round window, has often been injured too. The vestibular system and the inner ear are usually a “closed system” protected from changes in changes in outside air pressure by this thin membrane. If the vestibular system is open to outside air pressure, the fluid in the endolymphatic sacs in the semi-circular canals is fine when the barometric pressure is high on sunny days at low altitude. When the outside air pressure is low, or changing from high to low, the fluid in the endolymphatic system in the semicircular canals changes and the vestibular information from the injured ear disagrees with the information from the uninjured ear. This creates problems on rainy days and at altitude or in airplanes that are pressurized to 8,000 feet. The patient may experience anxiety, dizziness, disequilibrium, memory loss, nausea and a feeling of fullness in one or both ears.
Panic Attacks: The most primitive part of the brain is the part of the brain that requires accurate information about where it is in space. Some patients may have enough anxiety from their vestibular injury that they experience a “panic attack” in certain situations. Unless their physician is familiar with the effects of vestibular injuries, these panic attacks may be mis diagnosed as a psychiatric problem.
Sleep: The panic attacks may even occur during sleep. During sleep, the joint receptors don’t have gravity to give them information about position, the eyes are closed so there is no visual information and the brain has only the ears for information about where it is in space. The patient may fall asleep easily but after 60 to 90 minutes when they have to move to be comfortable, the two ears give the brain
conflicting information and the patient wakes up with a pounding heart and severe anxiety thinking that it is falling through space.
Legal Situations: Patients with vestibular injuries cannot pass a “field sobriety test” administered when a police officer stops a driver he suspects of drunk driving. The field sobriety test includes the instruction to “Follow my finger with your eyes” as the officer moves the finger horizontally from side to side. He is looking for bouncing in the eyes called saccades or nystagmus. A drunk driver will have bouncing of the eyes due to the effects of alcohol. A vestibular patient has bouncing of the eyes because of the vestibular injury. The field sobriety test may also include the instruction to perform some activity like walking heel to toe that demonstrates the ability to balance. Patients with vestibular injuries cannot perform these balance tests. It is a good idea to ask your physician for a note explaining the deficits created by your medical condition.
Treatment for Vestibular Injury Patients
There is no “cure” for vestibular injuries but there are ways of managing the symptoms and problems they create.
Medication to quiet the vestibular centers in the brain can help. Valium is the most effective prescription medication but is not used much because it is known to be addictive. Meclizine (Bonine) is a “non-drowsy”, over the counter motion sickness pill. It can be taken with two doses at bed time, and one dose in the morning and up to six doses in a day when air pressure is low.
Sleep with pillows on the chest, the back and between the knees to give the brain physical information about position (proprioception). Sleep with a dim night light on so that you can see where you are going and find a horizon when you have to navigate to the bathroom or anyplace else when the house is dark.
Label storage: Label the drawers and cupboards in the kitchen and bedroom so you know where to look for things that have been put away. This helps reduce the clutter on countertops and flat surfaces and allows you to put items away.
Create horizons: Arrange furniture, pictures, window shades in such a way as to create horizontal lines. This makes the eyes and brain more comfortable.
Prism Glasses: There are optometrists who are specially trained in the effects of vestibular injuries on visual function. They have an extra certification as a “Fellow of the College of Optometry and Visual Development” or FCOVD. You can search for such an optometrist by searching for an “FCOVD” near me. FCOVD optometrists prescribe special lenses with prisms to bend the light so it hits the retina in the right place to compensate for the lack of control of smooth pursuit created by the vestibular injury. The prism glasses make reading, driving and being in busy crowded places easier and reduces the symptoms from vestibular injuries. The prisms have to be exactly correct and the optometrist may have to adjust the lenses a few times to create an optimal response.
Some FCOVD optometrists prefer to provide “vision therapy” to train the eyes to be less sensitive to the vestibular mis-information. Vision therapy can be time consuming, expensive and can create symptoms that patients don’t tolerate well. My personal preference is that patients wear prism glasses for at least six months so they have a break from the vestibular symptoms and the brain has an idea about what “normal” is. Prism glasses can reduce the fatigue and nausea experienced by patients with vestibular injuries.
